What is Urinary Tract Obstruction?
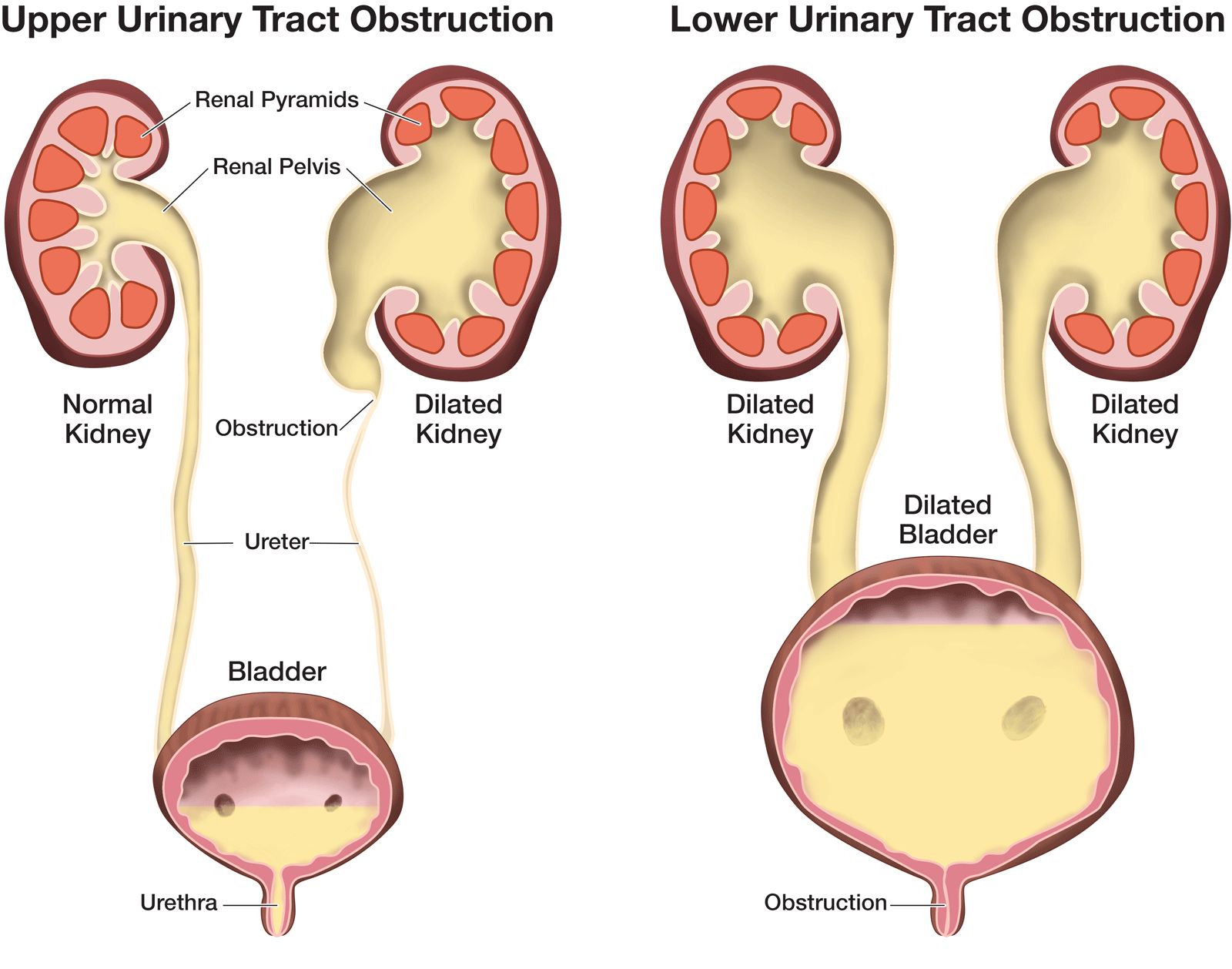
The urinary tract consists of two kidneys (where urine is made), two ureters (tubes which lead the urine into the bladder), the bladder, and the urethra (the tube which leads the urine from the bladder to the outside of the body). The urine should flow from the kidney, through the ureter, to the bladder, and out of the fetus through the urethra to the amniotic fluid. There are many causes of urinary tract obstruction in the fetus. Most are caused by a narrowing at some point in the urinary tract. This narrowing can slow down or stop the flow of urine, and this in turn can interfere with the development of both the kidneys and the lungs.
Amniotic fluid (fetal urine) is crucial in the development of the fetal lungs. If there is not enough amniotic fluid, the lungs of the fetus do not grow. As a result, fetal urinary tract obstruction can produce pulmonary hypoplasia (small lungs) and renal dysplasia (destruction of the kidneys). A low amniotic fluid level, or no amniotic fluid, can signal a blockage at some point in the urinary tract to the flow of urine.
What is the outcome for a fetus with urinary tract obstruction?
Outcome is related to the type of obstruction (where it is in the urinary tract), the severity of the obstruction, and the affect on renal function and amniotic fluid volume. Fetuses who have an obstruction or abnormality in one kidney and have a normal kidney on the other side will do very well. Individuals with one good kidney can support a normal life. All single-sided lesions, even those where the kidney is destroyed (dysplasia), can be successfully managed after birth. Fetuses with mild partial obstruction to both kidneys who do not have cysts in their kidneys or abnormal urine electrolytes and maintain their amniotic fluid volume can also be successfully managed after birth. It is important to follow these fetuses with serial ultrasound to make sure they maintain enough amniotic fluid volume for lung development and do not develop signs of kidney damage.
This is a good time to plan the time, type, and place of delivery. Although most babies will require some surgery after birth, it is usually not urgent. Most babies will not require intensive care and can be evaluated in the nursery or even later after they have left the hospital. However, fetuses with urinary tract obstruction that develop very dilated kidneys and have any degree of oligohydramnios and any risk of small lungs should be delivered in a specialized center with an intensive care nursery.
On the other end of the spectrum are fetuses with a blockage in the urinary system which does not allow the emptying of urine from either kidney. If the obstruction prevents urine from getting out into the amniotic space around the fetus, and the amniotic fluid goes away (oligohydramnios), the fetus’s lungs will not develop. The small lungs may prevent survival after birth. The obstruction also damages the kidneys, leading to kidney failure after birth. Many of these babies will not survive.
However, most fetuses with urinary tract obstruction fall between these two extremes and their outcome depends on the severity of the obstruction and how it progresses throughout the pregnancy. For all types of urinary tract obstruction, fetuses that lose all their amniotic fluid (oligohydramnios) before 18-24 weeks will not have big enough lungs to survive. Fetuses who maintain amniotic fluid volume throughout pregnancy will have large enough lungs to survive at birth, but may still develop renal failure after birth due to the damage to kidney function before birth. In addition to urologic procedures to relieve obstruction and sometimes reconstruct the urinary drainage system, these babies may develop renal failure over months or years and sometimes require kidney transplantation. Fetuses who maintain normal amniotic fluid and have only minor damage to the kidney will do well and may not need anything done after birth.
How serious is my fetus’s urinary tract obstruction?
Fortunately, the severity of damage to both the lungs and kidneys can often be determined by ultrasound and, sometimes, by sampling and analyzing the fetal urine. In most cases, serial ultrasound observation is all that is needed. This applies to all unilateral lesions in which there is one normal kidney. These fetuses can be safely followed by serial ultrasounds to make sure they maintain amniotic fluid volume and to help plan the delivery and care after birth.
Fetuses with obstruction to both kidneys must be closely followed for changes in amniotic fluid volume, further dilation of the urinary tract, and the sonographic appearance of the kidneys themselves (increased echogenicity or brightness suggests ongoing damage to the kidney itself). If amniotic fluid volume is maintained, the kidney echogenicity does not deteriorate, and the system does not become more dilated, then these fetuses can be followed to normal delivery near term and treatment after birth. Some may require several surgeries after birth, but most will do well.
Fetuses with obstruction to both kidneys, dilated bladder and ureters, and increasing echogenicity of the kidney itself, are on the severe end of the spectrum and some will not survive. Very severely affected fetuses, who lose amniotic fluid before 18 weeks of gestation and have very echogenic, dysplastic, or multicystic kidneys, often cannot be saved. When these symptoms take place fetal urine will show a salt content which demonstrates that the kidneys cannot function properly.
Fetuses with obstruction to both kidneys that has not caused increased echogenicity or dysplasia and who have maintained the kidneys’ ability to extract salt from the urine, may be saved by fetal intervention to relieve the urinary tract obstruction. These fetuses should be carefully studied for the degree of renal dysplasia or echogenicity, for the degree of dilation of the urinary tract and the anatomy of the obstruction, either at the bladder outlet or above the bladder, and for the amniotic fluid volume. Those who are candidates for fetal intervention can be accurately assessed for the degree of renal functional damage by sampling and testing the fetal urine 2–3 times over 3–5 days to measure fetal urine electrolytes and beta-2-microglobulin. These tests are quite accurate in predicting how well the fetal kidneys are functioning, the degree of impairment, and the potential to recover.
What are my choices during this pregnancy?
In cases where the urinary obstruction affects both kidneys and there is low or absent amniotic fluid, a careful and thorough evaluation is necessary because fetal intervention may be an option.
Prior to fetal intervention, it is essential to determine that the kidneys have not suffered damage that would make normal function impossible. There are two ways that kidneys can be assessed. The first is by ultrasound evaluation. The radiologist can determine on an ultrasound whether or not the kidney tissue looks normal. The presence of cysts or echogenic (bright white) tissue is usually not a favorable sign.
The second method of determining kidney function in a fetus is by taking a sample of fetal urine and analyzing the electrolytes and protein levels. This procedure is done exactly like an amniocentesis. A needle is placed through the mother’s abdomen and into the fetus’s bladder. A fetal urine sample is taken, the fetal bladder is completely drained of urine, and the urine sample is sent for testing. Determination of normal karyotype (chromosomes) can also be done on this urine sample of the fetus. This procedure should be repeated in 24 to 48 hours and the fetal urine should again be sent for electrolytes and protein. It may be necessary to take a third urine sample in another 24-48 hours. A fetal urine sample is taken three times in order to get the most accurate assessment of kidney function, as the first sample has been in the bladder for a long time and may not give the best information. The second sample may be urine which had been in the kidneys for a prolonged period of time and drained into the bladder after the first bladder tap. The results of the analysis on the third sample enable the medical team to give the most accurate prognosis and recommendations for treatment. Only fetuses with bilateral (both kidneys) urinary obstruction and evidence of good kidney function by ultrasound and electrolyte and protein levels are candidates for fetal intervention.
Fetuses with bilateral obstructions (usually males with posterior urethral valves) who lose amniotic fluid volume and develop signs of renal compromise before 24 weeks, require intensive management before and after birth.
The most severe cases have evidence of progressive renal failure. The kidneys show cysts or increased “brightness” (echogenicity), urine electrolytes are abnormal, and amniotic fluid may decrease or disappear. These fetuses may require decompression, relief of the obstruction, before birth.
Fetal Intervention
The goal of fetal intervention is to allow the urine to get past the obstruction. Restoring the normal flow of urine into the amniotic fluid will allow the lungs to grow and the kidneys to develop. Fetal intervention for urinary obstruction has improved dramatically over the past 25 years. The first fetal intervention for urinary obstruction involved open fetal surgery (an incision in the uterus to expose the fetus) and placement of a vesicostomy (an opening to the fetal bladder). This method of treatment was successful, but the women who underwent this procedure experienced preterm labor from the incision made in the uterus.
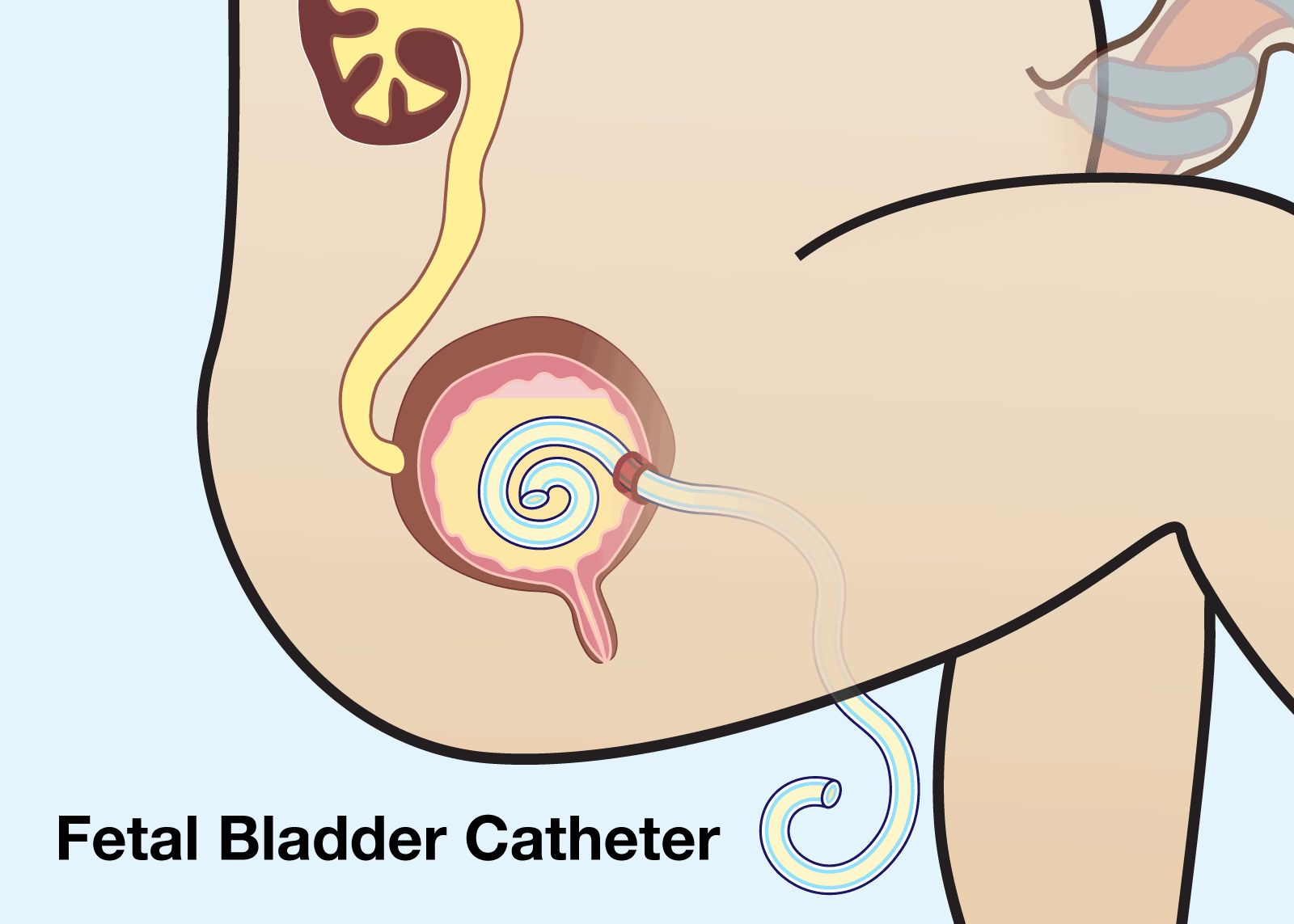
Fetal Bladder Catheter
To solve the problems with open fetal surgery, a less invasive intervention was developed using the placement of a specially designed tube, the Harrison Catheter, into the fetal bladder. The procedure is similar to an amniocentesis. A small hollow needle is placed through the mother’s abdomen into the fetal bladder, using the sonogram for visualization. One end of the tube is in the fetal bladder and the other end in the amniotic fluid. Urine escapes the fetal bladder through the tube. This technique has proven effect and has been used thousands of times around the world with good success. However, it is difficult to keep these little tubes in place and functioning for extended periods of time as they can become plugged or dislodged, sometimes requiring repeated procedures.
Minimally Invasive Surgery
More recently, we have developed a technique (FETENDO fetal surgery) to directly relieve the obstruction at the bladder outlet by putting a very small (3-mm) fetoscope directly into the fetal bladder and disrupting the valves, opening the obstruction. This can now be done through a very small scope placed through a small incision in the mother’s skin rather than through open surgery. Relieving fetal urinary tract obstruction has proven very effective in restoring amniotic fluid volume and allowing the fetal lungs to grow. It is not yet proven that relieving the obstruction before birth will always preserve renal function and prevent long-term renal failure.
What will happen after birth if only one kidney has a problem?
We recommend that after consulting with your primary physician, your newborn be started on Amoxicillin, an antibiotic, immediately after birth. This will prevent any infection of the urinary tract. No testing is recommended until the baby is one month of age and the kidney function has matured. At this time, we would recommend a renal (kidney) ultrasound and a Diuretic Renal Scan, and an appointment with a pediatric urologist for consultation. Both of these tests will help evaluate the anatomy and function of the kidneys.
On occasion, the urologist will request a third test, called a “Voiding Cystourethrogram” or VCUG, to examine the urinary system for reflux (or back up) of urine from the bladder into the kidneys. Based on the results of these studies, the urologist will be able to identify the specific renal abnormality, assess the health of the kidney(s), and make recommendations for the treatment of your baby’s condition. The recommendations for treatment range from periodic testing to operation intervention.
Support Groups & Other Resources
- The Fetal Hope Foundation — provides support and information to parents, funds research, and increases awareness about TTTS, TRAP Sequence, Amniotic Band Syndrome, and Urinary Tract Obstruction
- March of Dimes — Researchers, volunteers, educators, outreach workers and advocates working together to give all babies a fighting chance
- Birth Defect Research for Children — a parent networking service that connects families who have children with the same birth defects
- Kids Health — doctor-approved health information about children from before birth through adolescence
- CDC - Birth Defects — Dept. of Health & Human Services, Centers for Disease Control and Prevention
- NIH - Office of Rare Diseases — National Inst. of Health - Office of Rare Diseases
- North American Fetal Therapy Network — NAFTNet (the North American Fetal Therapy Network) is a voluntary association of medical centers in the United States and Canada with established expertise in fetal surgery and other forms of multidisciplinary care for complex disorders of the fetus.