UCSF is the premier center for the diagnosis and management of pregnancies with hydrops. We have decades of experience with hydrops and offer cutting-edge genomic testing, fetal imaging, comprehensive prenatal and neonatal care, and access to novel in utero treatments. Our approach to care is multidisciplinary, with internationally recognized experts from Maternal-Fetal Medicine, Genetics, Radiology, Pediatric Surgery, Neonatal Medicine, Pediatric Cardiology, and many other subspecialities who work together to provide the best, individualized care for each patient.
What is Hydrops?
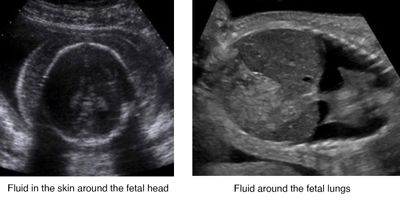
Hydrops is a condition in pregnancy marked by abnormal collections of fluid in the developing fetus (such as fluid around the lungs or the heart, in the abdomen, or in the skin). Hydrops can develop at any point during pregnancy, and many genetic diseases that underlie hydrops can present early in pregnancy with a cystic hygroma or later with multiple abnormal fluid collections. Hydrops presents risks to both the pregnant individual and the fetus. These include preterm birth, stillbirth, preeclampsia, and potentially, major illness or death for the newborn.
There are two types of hydrops: one is immune and results from differences in the blood between a pregnant individual and the fetus, while the other is non-immune and results from many genetic and viral causes. Because most cases of immune hydrops (also referred to as alloimmunization) can be prevented with RhoGAM, non-immune hydrops is the most common type of hydrops seen today. Hydrops can also occur in the setting of twin-twin transfusion syndrome, which is a separate condition that is treated differently.
Immune Hydrops (Alloimmunization)
Immune hydrops results from differences in the blood between a pregnant individual and fetus. These differences can cause a pregnant person to develop antibodies to small molecules on the fetus’ red blood cells. These antibodies can then cross the placenta, leading to a low red blood cell count in the fetus (anemia), which can in turn lead to hydrops. In most cases, but not all, RhoGAM can be given during pregnancy to prevent immune hydrops. Both fetal anemia and immune hydrops are treated with in utero transfusions that deliver blood to the fetus through the umbilical cord.
Non-Immune Hydrops
Non-immune hydrops can develop in pregnancies where the fetus has an underlying genetic disease or when a viral infection occurs. Genetic diseases presenting with hydrops may result from chromosome imbalances or small variations within a single gene. Our HyDROPS research group has identified a number of genetic diseases underlying cases of non-immune hydrops, such as Turner syndrome, Noonan syndrome, alpha thalassemia major, Milroy disease, mucopolysaccharidosis type VII, Diamond Blackfan anemia, and many others. For a more detailed discussion about genetic diseases that can present with hydrops we recommend watching our video Genetic Diseases Linked to Nonimmune Hydrops
Standard genetic testing (using karyotype or microarray) will miss variations at the level of a single gene, leaving the reason for hydrops unexplained in many cases. However, at UCSF, we have pioneered the use of prenatal exome sequencing to identify single gene variations and provide an explanation for hydrops and other birth defects (Exome Sequencing for Prenatal Diagnosis in Nonimmune Hydrops Fetalis. N Engl J Med 2020).
The treatment for non-immune hydrops is dependent on the underlying cause. Examples of interventions that may be recommended are in utero transfusions, placement of a shunt, or consideration of novel fetal treatments in development at UCSF such as in utero enzyme replacement therapy.
Excellence in Hydrops Care at UCSF
The diagnosis and management of hydrops is complex. UCSF brings extensive experience, cutting-edge diagnostics, and novel approaches to the treatment for hydrops.
- Personalized genomics: Genomic sequencing is available through the UCSF Genomic Medicine Laboratory. The lab has extensive experience with genes involved in the development of hydrops, and the details of every case are reviewed by an expert, multidisciplinary panel. We provide personalized genetic counseling to discuss the sequencing and how the results affect current and future pregnancies.
- Detailed prenatal imaging: Internationally recognized experts at UCSF use advanced imaging tools to identify subtle clues that may reveal the reason for hydrops. This imaging is performed with prenatal ultrasound, and in many cases with MRI as well.
- State-of-the-art fetal procedures: The full range of clinically indicated fetal procedures for hydrops is offered by experienced clinicians in the Fetal Treatment Center at UCSF, including fetal shunts, laser therapy, and in utero transfusions. We also offer access to clinical trials of novel fetal therapies such as in utero stem cell transplantation and enzyme replacement therapy. A multidisciplinary team of fetal medicine and surgical experts reviews every case to determine the best approach for each pregnancy.
- Novel fetal therapies: Dr. Tippi MacKenzie oversees clinical trials of in utero stem cell transplantation (Clinical Trial: NCT02986698) for alpha thalassemia major and enzyme replacement therapy (Clinical Trial: NCT04532047) for a group of genetic diseases referred to as inborn errors of metabolism. The goal of these phase 1 clinical trials is to treat genetic diseases in utero to improve their outcomes after birth.
- Comprehensive perinatal care: Our team of experts spans many prenatal and pediatric subspecialties and prepares individualized, comprehensive perinatal care plans for each patient. These plans may include imaging surveillance during pregnancy, fetal interventions, special considerations for delivery, subspecialists needed at delivery, neonatal treatments, and more.
- Mental health and emotional support: Patients have access to Social Work and Palliative Care providers, who are specially trained to care for families with difficult pregnancies and perinatal loss.