What is Twin to Twin Transfusion Syndrome (TTTS)?
Because there is no barrier separating the two fetuses from each other, there are almost always blood vessel connections in the placenta shared by two fetuses in monochorionic twin (MC) pregnancies. As a result of these connections, in about 10-15% of monochorionic twins (sharing one placenta) an imbalance in the circulations of the fetuses can develop. In these instances, there may be significant transfer of blood from one twin (the so-called “donor”) to the other twin (the so-called “recipient”), resulting in twin-to-twin transfusion syndrome (TTTS).
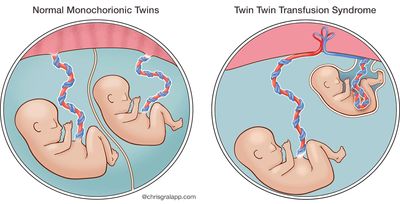
Twin-to-Twin Transfusion Syndrome (TTTS) is a serious, progressive disorder. The twins do not have malformations, but one transfuses the other through abnormal or imbalanced blood vessel connections in the shared placenta. More specifically, an artery branches off from the donor twin’s umbilical cord, entering the placenta in order to obtain oxygen and nutrients for the blood from the mother’s circulation. Unfortunately, the corresponding vein that would normally bring the now nutrient-rich blood back to that same fetus instead is directed toward the other twin via this abnormal “arterio-venous” connection. As a result, if there are no connections flowing in the opposite direction, one twin receives too much blood and the other too little.
Twin to Twin Transfusion Presentation Part 1
Twin to Twin Transfusion Presentation Part 2
How Does This Blood Imbalance Affect the Fetus?
When a fetus is anemic, or doesn’t have enough blood and oxygen, it tries to use what it has most efficiently. This is accomplished by emphasizing the blood flow to the most important organs (the brain and the heart) and shutting down less vital organs, such as the kidneys. Thus, the ‘donor’ twin will make a lot less — and sometimes no — urine. Meanwhile, the recipient twin is overloaded with blood and volume, and is urinating excessively as a result.
Low amniotic fluid is termed “oligohydramnios”, while a high level of amniotic fluid is called “polyhydramnios”. TTTS is diagnosed by the ultrasound findings of high amniotic fluid (polyhydramnios) in the amniotic sac of one twin (the recipient) and low amniotic fluid (oligohydramnios) around the other twin (the donor). The recipient’s blood can become thick and difficult to pump around the body. The recipient twin, having to pump the thick extra volume of blood, can develop heart failure, generalized soft tissue swelling (“hydrops”), and, in some cases, fetal death.
The donor twin is at risk for developing failure of the kidneys and other organs because of inadequate blood flow. Because of the blood vessels that connect the circulations of the two fetuses across the shared placenta, if one twin dies, the other twin faces significant risk of death or damage to vital organs. If the other twin survives, there is up to a 40% risk of some form of brain injury. Unfortunately, without treatment, approximately 70–80% of twins with TTTS will die. Survivors may have injuries to their brains, hearts and/or kidneys.
Although technically speaking the diagnosis of TTTS is based on the amniotic fluid levels in each sac, the twins may be significantly different in their weights/sizes as well. Some of the size differences may be due to the TTTS process. However, much of the difference in size results from the fact that the portion of the placenta devoted to each twin differs (unequal placental sharing). The majority of MC twins that develop TTTS also have some unequal placental sharing, with smaller placental portion assigned to the donor twin. Further, many twins that only have unequal placental sharing (but are not transfusing one another) may be incorrectly diagnosed as having TTTS. Differences may be subtle, but outcomes are dependent on accurate diagnosis, and the treatment and management are different for these conditions.
What is the outcome for a fetus with TTTS?
In Twin-to-Twin Transfusion Syndrome (TTTS), the donor twin responds to anemia and low volume by trying to make the most efficient use of the blood it does have. Blood is shunted preferentially to the most vital organs (the brain and the heart), and away from other, less vital, internal organs such as the kidneys. This partial shutdown of the kidneys results in the fetus making less urine. Because amniotic fluid is mostly comprised of fetal urine, the reduced urine output results in low amniotic fluid level, or ‘oligohydramnios’.
As the kidneys make less and less urine and the degree of oligohydramnios worsens, the fetal bladder may become empty and no longer visible by ultrasound (as it is not being filled with urine). Meanwhile, the recipient becomes overloaded with fluid as a result of the on-going blood transfusion from the donor twin, and responds by producing large amounts of urine in an effort to reduce all of its excess volume. This leads to very large amounts of amniotic fluid in the recipient’s sac (“polyhydramnios”). It is the combination of oligohydramnios and polyhydramnios in a MC twin pair seen by ultrasound that indicates the diagnosis of TTTS. Careful obstetric ultrasound is crucial for correctly detecting and diagnosing TTTS during pregnancy. The ultrasound exams at our center are performed by specialists, widely renowned for their diagnostic skills and expertise in this field, who have written textbooks and many scientific articles about fetal conditions, such as TTTS and unequal placental sharing.
In cases of TTTS, in addition to abnormal amniotic fluid volumes, the twins are often discrepant in size as well, with significant discordance in their estimated fetal weights. The recipient’s blood can become thick and difficult to pump around the body. The recipient twin, having to pump the thick extra volume of blood, can develop heart failure, generalized soft tissue swelling (“hydrops”), and, in some cases, fetal death. The donor twin is at risk for developing failure of the kidneys and other organs because of inadequate blood flow. Because of the blood vessels that connect the circulations of the two fetuses across the shared placenta, if one twin dies, the other twin faces significant risk of death or damage to vital organs. If the other twin survives, there is up to a 40% risk of some form of brain injury. Unfortunately, without treatment, approximately 70–80% of twins with TTTS will die. Survivors may have injuries to their brains, hearts and/or kidneys.
Maternal Mirror Syndrome
In cases with extreme fetal tissue swelling, or “hydrops”, the pregnant woman may be at risk for maternal “mirror” syndrome, the term used to describe the process in which the mother’s condition mimics that of the sick fetus. Because of a high-flow, high-volume cardiovascular state, the mother may develop symptoms that are similar to pre-eclampsia — which may include vomiting, hypertension, generalized body swelling (more so than usual), excessive protein in the urine (proteinuria), and dangerous build-up of fluid in her lungs (pulmonary edema). While this is a rare occurrence, it is imperative that the pregnant woman be carefully followed. Management must include continued optimal obstetric/prenatal care with surveillance for such maternal conditions, while attention is paid to the complicated twin pregnancy.
How serious is my fetus’s condition?
The severity of Twin-to-Twin Transfusion Syndrome (TTTS) is partially based on the stage in pregnancy at which the condition becomes evident (the earlier it presents, the more serious it is). In addition, the degree of fluid imbalance between the twins is important in grading or staging the problem. True TTTS occurs when one twin of a monochorionic pair is shown by ultrasound to have a deepest pocket of amniotic fluid in its sac of less than 2cm (the donor), while at the same time, the deepest pocket of amniotic fluid measures greater than 8cm in the other twin’s sac (the recipient).
A bladder that remains empty in the donor twin is a concerning sign, indicating a more advanced stage of TTTS. The situation worsens further when, in addition to abnormal discrepant fluid volumes, abnormal blood flow patterns are shown by ultrasound in the umbilical cord vessels of either or both twins. Finally, evidence of heart failure and tissue swelling (hydrops) in either twin, usually the recipient, is an indication of a very serious, advanced stage.
Dr. Ruben Quintero developed the widely used staging system for TTTS (see below). Many patients in whom TTTS is suspected may, on further investigation, be found to have twins with discrepant fluid volumes but do not meet the definition for stage I TTTS. Still, all patients carrying MC twins with significantly unequal amniotic fluid volumes and/or fetal weights should be evaluated and followed very carefully for changes, as true TTTS can develop and worsen rapidly.
Fetal Echocardiogram
To further evaluate the severity of TTTS, fetal echocardiography is often performed at our institution. Fetal echocardiograms are specialized, targeted ultrasound studies of the heart, performed by pediatric cardiologists with special expertise in this area.
Early changes of heart failure are usually seen first in the recipient twin, as its heart has to work hard to pump the extra blood. These exams may reveal increased size of some of the heart chambers, and changes in flow across the heart valves (for example, tricuspid regurgitation). If the stress and overload on the recipient continues untreated, progressive changes may include decreased function of the heart chambers, and possible development of narrowing of one of the heart valves (pulmonary stenosis).
Umbilical Artery Blood Flow
Finally, using information from both the echocardiogram and obstetric ultrasound exam, we look for blood flow patterns in the umbilical artery and vein and other major fetal blood vessels. Blood in the umbilical artery (UA) normally flows away from the fetus and toward the placenta, in an attempt to obtain fresh oxygen and nutrients from the mother’s circulation. If a placental condition worsens, it becomes harder for the blood to flow toward and within the placenta. With each heartbeat, the fetus pushes blood toward the placenta (the systole phase) through the umbilical artery, and normally, that beat is strong enough for blood to keep flowing forward, toward the placenta, even as the heart re-fills for its next beat (the diastole phase).
In some cases, as TTTS progresses, forward flow in the umbilical artery of the donor may diminish between heartbeats. If the condition worsens, there may be no flow or even reversal of flow direction during the re-filling (diastole phase) of the fetal heart.
All of the echocardiogram and ultrasound exam findings are considered in determining the severity of TTTS for each individual pregnancy.
What treatment choices do I have and is laser the only option?
Because Twin-to-Twin Transfusion Syndrome (TTTS) is a progressive disorder, early treatment may prevent complications, including preterm labor and premature rupture of membranes due to excessive fluid (polyhydramnios). Treatment for TTTS depends on the severity of the condition and the current stage of your pregnancy.
Fetoscopic Laser Intervention
All patients with stage II, III or IV TTTS—and some patients with stage I—should learn about and consider fetal intervention. In most instances, the appropriate, optimal therapy will be fetoscopic laser intervention. Our center was one of the first in the world to perform fetoscopic laser to treat TTTS. Survival rates for at least one twin are greater than 85% and for both twins is approximately 60% at our center.
The fetal laser procedure is performed by introducing a thin fiber-optic scope through the mother’s abdominal wall, through the wall of the uterus and into the amniotic cavity of the recipient twin. By examining the blood vessels on the placental surface directly, the abnormal vascular connections between the twins can be found and eliminated by directing a laser beam at them. Only those vessels that go from one twin to the other are coagulated by the laser beam. The normal blood vessels that help nourish each twin are left intact.
A detailed ultrasound examination prior to the procedure demonstrates the sites where the umbilical cords attach to the shared placenta and may help locate abnormal inter-twin connections, making it quicker and easier to identify with the fetoscope. After the laser procedure is completed, an amnioreduction (removing extra amniotic fluid) is performed, to decrease the chance of early labor and help make the pregnancy more comfortable.
What About Amnioreduction?
Many families ask whether amnioreduction is a potential treatment option for TTTS. Some of our most expert European colleagues attempted to address the question whether laser or amnioreduction was the best therapy for TTTS. In a randomized prospective trial, they found 76% survival of at least one fetus and 36% survival of both twins with laser, compared with 51% survival of at least one fetus and 26% survival of both twins with amnioreduction. For many researchers and experts in this field, this study showed that laser was the preferred therapy for TTTS.
At our center, however, we have found a group of patients with early TTTS that respond well to amnioreduction, a less invasive therapy. In a small percentage of pregnancies that develop TTTS, an artery to artery (A-A) connection between the twins on the surface of the placenta can be found using ultrasound. The twin-pairs in whom these connections are demonstrated by ultrasound, have been shown to have better outcomes overall, and in our experience, over 80% survival of both twins after being treated with amnioreduction. Thus, although laser is the appropriate therapy for the vast majority of patients with TTTS, we occasionally offer amnioreduction to patients with TTTS who meet criteria for this therapy.
With our multidisciplinary team of expert radiologists and surgeons the Fetal Treatment Center is uniquely qualified to evaluate which treatment is best for you. To find out more best please contact our center: 1-800-RX-FETUS.
Support Groups & Other Resources
- San Francisco Parents of Multiples Club — a network of parents and expectant parents of multiples that provides its members and their families with friendship, support and information on parenting twins, triplets and quads.
- The Fetal Hope Foundation — provides support and information to parents, funds research, and increases awareness about TTTS, TRAP Sequence, Amniotic Band Syndrome, and Urinary Tract Obstruction.
- TTTS Foundation — solely dedicated to providing immediate and lifesaving educational, emotional and financial support to families, MDcal professionals, and other caregivers before, during, and after a diagnosis of twin to twin transfusion syndrome.
- March of Dimes — Researchers, volunteers, educators, outreach workers and advocates working together to give all babies a fighting chance
- Birth Defect Research for Children — a parent networking service that connects families who have children with the same birth defects
- Kids Health — doctor-approved health information about children from before birth through adolescence
- CDC - Birth Defects — Dept. of Health & Human Services, Centers for Disease Control and Prevention
- NIH - Office of Rare Diseases — National Inst. of Health - Office of Rare Diseases
- North American Fetal Therapy Network — NAFTNet (the North American Fetal Therapy Network) is a voluntary association of medical centers in the United States and Canada with established expertise in fetal surgery and other forms of multidisciplinary care for complex disorders of the fetus.