What is TRAP sequence or acardiac twin?
Twin reversed arterial perfusion (TRAP) sequence or acardiac twinning is a very rare problem, occurring in approximately 1% of monochorionic twins (MC, twins sharing one placenta). One twin is usually structurally completely normal. The other is an abnormal mass of tissue, consisting usually of legs and a lower body, but no upper body, head or heart. Because of the absent heart, the term “acardiac twin” has been used to describe this mass. The normal fetus is referred to as the “pump twin” because its heart is used to pump blood to the abnormal mass. The “acardiac twin” has no chance of survival.
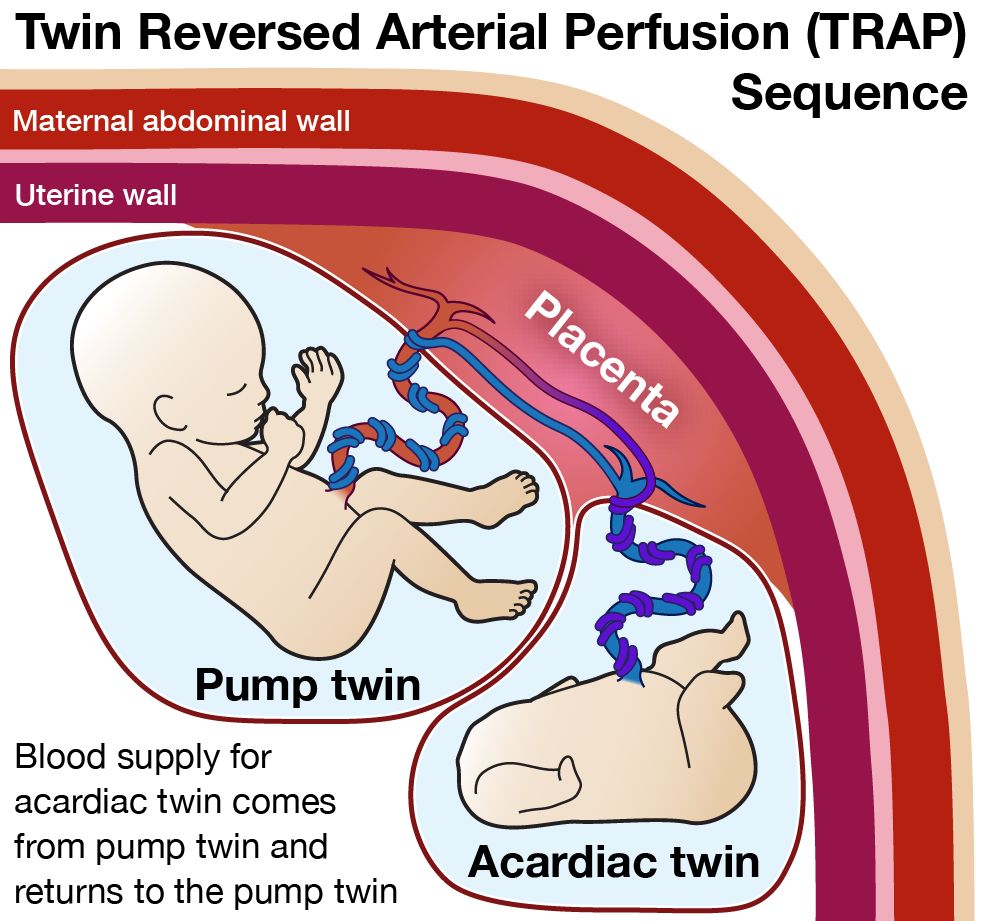
Due to the absence of a beating heart, the acardiac does not send blood to any portion of the placenta, and all of its blood supply comes from and goes back to the circulation of the pump twin through unique vascular connections on the surface of the shared placenta. Arteries usually carry blood away from the fetus and toward the placenta to receive oxygen from the mother’s circulation. When there is an “acardiac twin”, the unique vascular connections allow blood in the artery to flow in the reversed direction (toward the acardiac fetus rather than away from it). Thus, the phrase “twin reversed arterial perfusion” (TRAP) sequence has been used to describe this condition.
The normal “pump” twin faces the excess burden of having to send and receive blood to the acardiac mass as well as to its own growing tissues. As such, the normal twin’s heart has to work extra hard and is under a lot of stress. This can result in heart failure for the normal twin. Left untreated, up to 50% of these otherwise normal twins may die in utero (stillbirth) or die shortly after birth.
How serious is my fetus’s condition?
The risk of the normal or pump twin going into heart failure and dying seems to depend on the size of the acardiac. The larger the acardiac compared to the pump twin the greater the risk. The amount of blood flow into the acardiac also seems to play a role. The more blood flow the higher the risk. The harder the pump twin's heart is working, the greater the risk of heart failure also. All of these things can be followed with ultrasound and echocardiography. In cases of a large acardiac, these tests may have to be repeated frequently.
What options do I have?
Pregnancy Monitoring
Cases where the acardiac twin is small and there is little cardiac stress on the pump twin can be monitored by ultrasound. With frequent ultrasounds, we can follow the health of the normal twin and identify signs of heart failure. If heart failure of the pump twin is identified, and the pregnancy is in the third trimester then the normal pump twin would simply be delivered.
In high risk cases where there is high blood flow to the acardiac twin it may begin to cause too much strain on pump twin's heart. Impending heart failure may be an indication for fetal intervention.
Fetal Treatment
In cases high risk cases, we use a method of selective termination, safely stopping flow to the acardiac mass. This way the normal pump twin is protected and is no longer in danger of heart failure or death.
Support Groups & Other Resources
- San Francisco Parents of Multiples Club — a network of parents and expectant parents of multiples that provides its members and their families with friendship, support and information on parenting twins, triplets and quads.
- The Fetal Hope Foundation — provides support and information to parents, funds research, and increases awareness about TTTS, TRAP Sequence, Amniotic Band Syndrome, and Urinary Tract Obstruction.
- TTTS Foundation — solely dedicated to providing immediate and lifesaving educational, emotional and financial support to families, MDcal professionals, and other caregivers before, during, and after a diagnosis of twin to twin transfusion syndrome.
- March of Dimes — Researchers, volunteers, educators, outreach workers and advocates working together to give all babies a fighting chance
- Birth Defect Research for Children — a parent networking service that connects families who have children with the same birth defects
- Kids Health — doctor-approved health information about children from before birth through adolescence
- CDC - Birth Defects — Dept. of Health & Human Services, Centers for Disease Control and Prevention
- NIH - Office of Rare Diseases — National Inst. of Health - Office of Rare Diseases
- North American Fetal Therapy Network — NAFTNet (the North American Fetal Therapy Network) is a voluntary association of medical centers in the United States and Canada with established expertise in fetal surgery and other forms of multidisciplinary care for complex disorders of the fetus.