What is Pulmonary Sequestration?
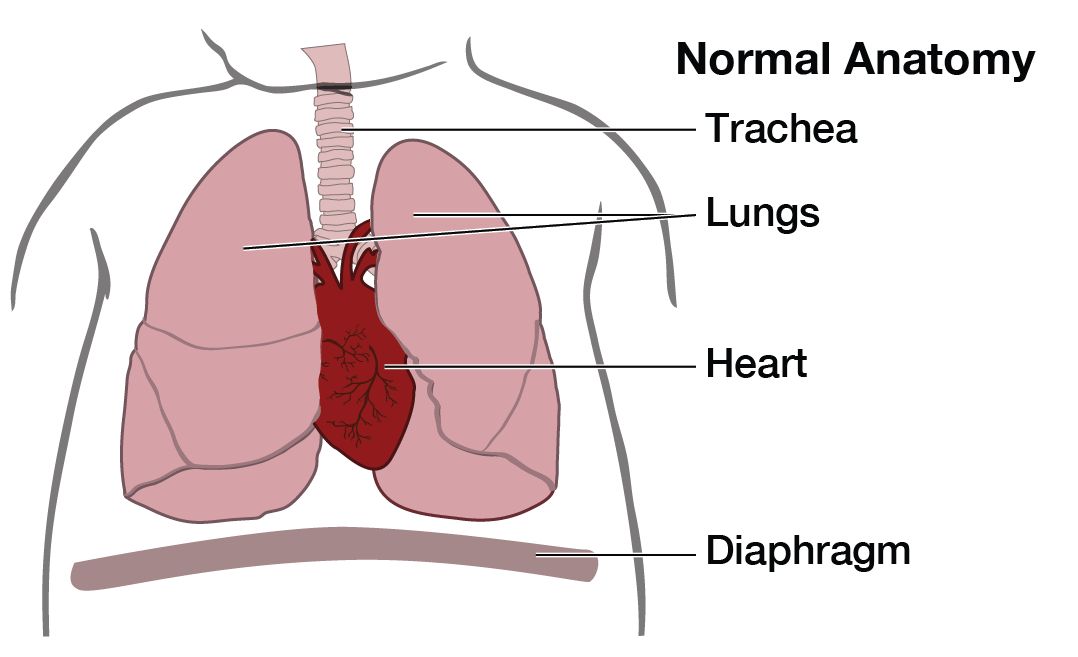
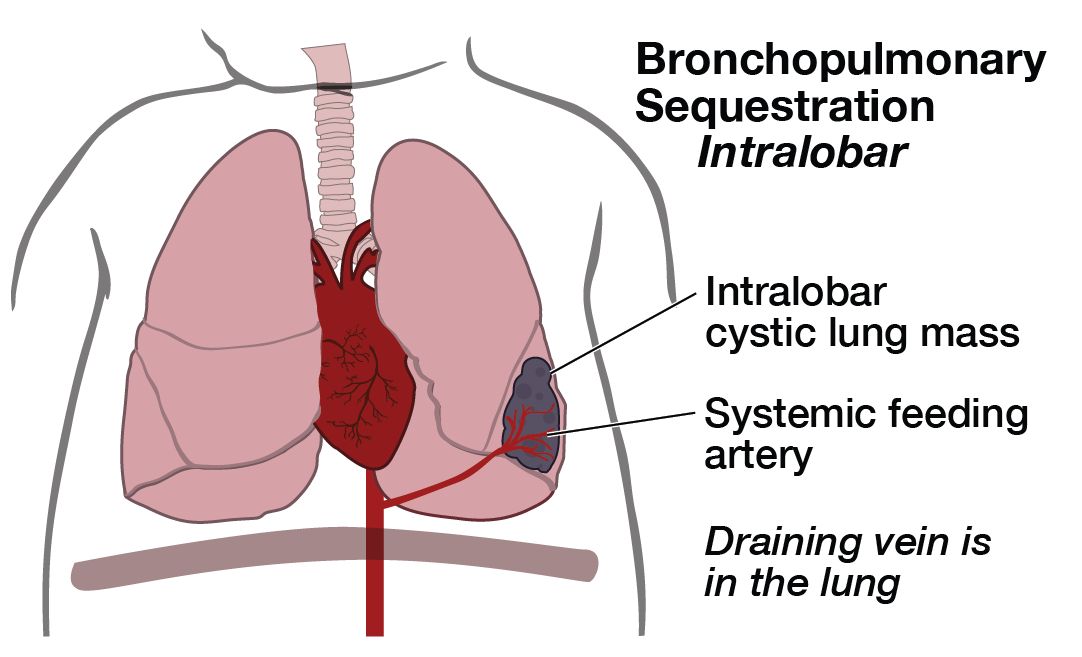
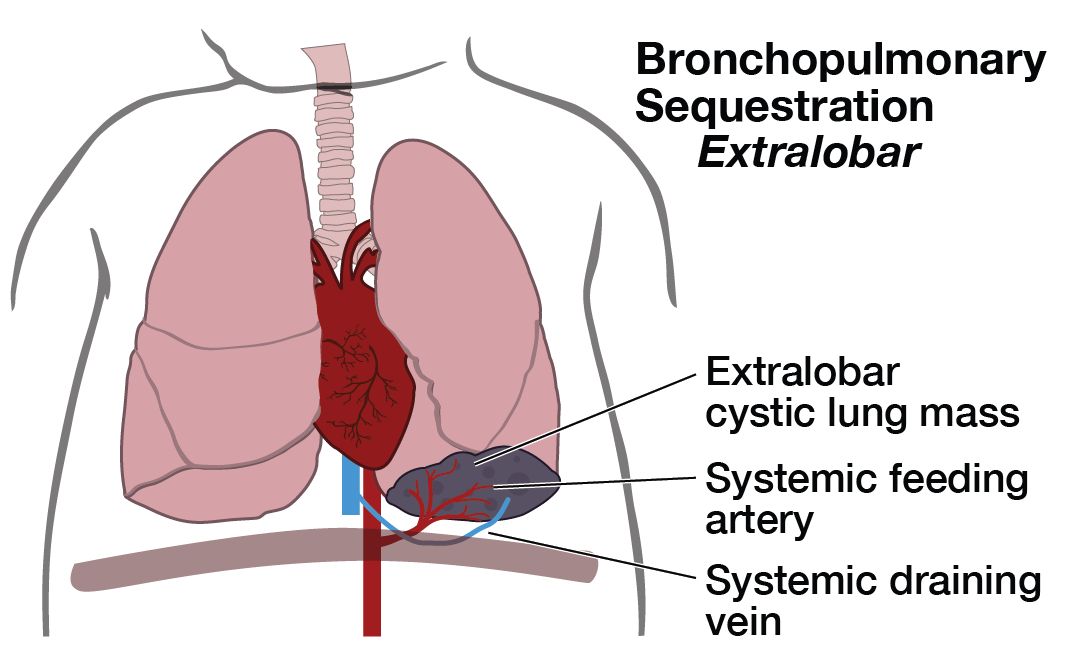
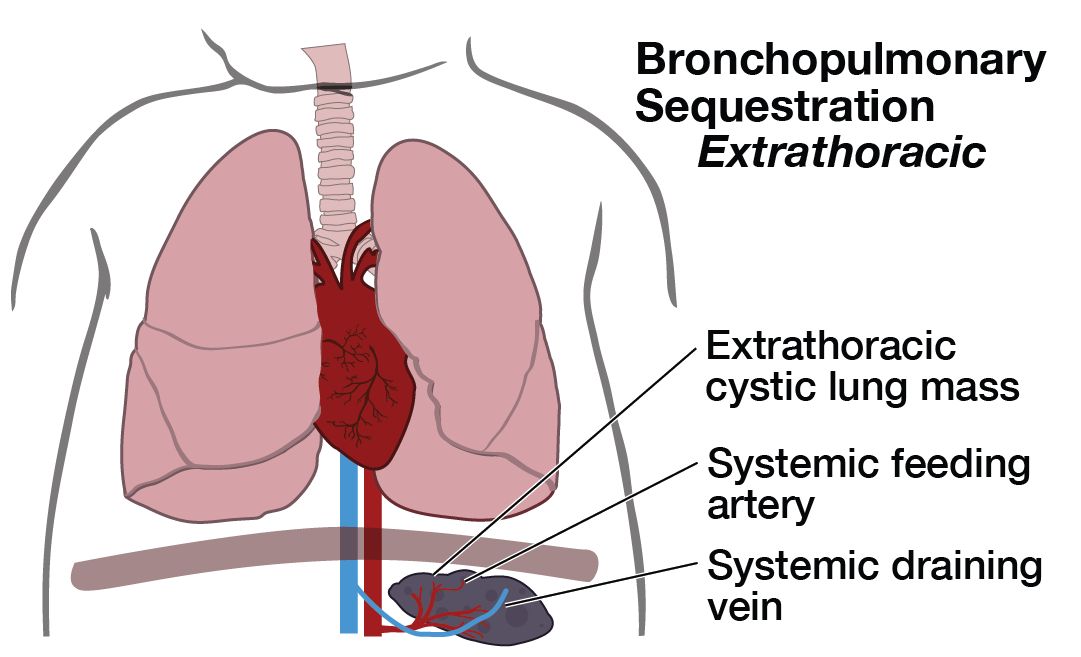
A pulmonary sequestration (also known as bronchopulmonary sequestration) is a cystic piece of abnormal lung tissue that does not work like normal lung tissue. They usually appear next to the lung (extrapulmonary, aka extralobar sequestration) or within one part of the lung (intrapulmonary, aka intralobar sequestration). We do not know what causes one part of the lung to develop abnormally. The cystic tissue involved will never function as normal lung tissue.
There are several types of cystic lung lesions including Congenital Pulmonary Airways Malformation CPAM (aka, congenital cystic adenomatoid malformation CCAM), pulmonary sequestration, and defects that are a mixture of these two. The abnormal piece of lung can be microcystic (many small cysts) or macrocystic (several large cysts). Pulmonary sequestrations are distinguished from CPAMs by the presence of a blood vessel that comes directly from the main artery (aorta) into the lung mass.
What is the outcome for a fetus with pulmonary sequestration?
Pulmonary sequestrations vary in size at presentation and can change throughout the pregnancy. The diagnosis is made by prenatal ultrasonographic findings of an echogenic (bright) mass appearing in the chest of the fetus. The mass may displace the heart from its normal position or push the diaphragm downward, but the key feature of a sequestration is the finding of an artery leading from the cystic mass directly to the aorta. This is what distinguishes a pulmonary sequestration from a CPAM.
The majority of these fetuses have a very good outcome. Pulmonary sequestrations remain the same size or grow with the fetus, but usually do not cause severe problems, probably because there remains enough room for the normal part of the lung to grow. The mass may shrink in size before birth. In all these cases, the outlook for a normal life is excellent. These fetuses should be followed closely, delivered near term, and the pulmonary sequestration removed surgically after birth — often the removal is an elective proceedure in early childhood.
Those who do not have hydrops when the lesion is first detected must be closely followed by doing ultrasounds at regular intervals to look for the development of hydrops. If fetuses do not develop hydrops, we continue a “wait-and-see” attitude with close follow-up. Many of these lesions will begin to decrease in size before 28 weeks of gestation and almost all can be safely treated after birth at a tertiary center.
A small number of fetuses with pulmonary sequestrations may develop large pleural effusions (excess fluid in the chest cavity) and even signs of heart failure (hydrops). Unlike CPAM that cause trouble by virtue of their size, pulmonary sequestrations threaten the fetus due to high blood flow through the lesion from the aorta. These are the only fetuses who are candidates for treatment before birth.
Maternal Mirror Syndrome
In cases with extreme fetal hydrops, the mother may be at risk for maternal mirror syndrome, which is a condition where the mother's condition mimics that of the sick fetus. Because of a hyperdynamic cardiovascular state, the mother develops symptoms that are similar to pre-eclampsia and may include vomiting, high blood pressure, swelling of the hands/feet/ankles, protein in the urine, or fluid in the lungs. Despite treatment of the anomaly, maternal mirror syndrome may still occur.
How serious is my fetus’s pulmonary sequestration?
In order to determine the severity of your fetus's condition it is important to gather information from a variety of tests and determine if there are any additional problems. These tests along with expert guidance are important for you to make the best decision about the proper treatment.
This includes:
- The type of defect—distinguishing it from other similar appearing problems.
- The severity of the defect—is your fetus’s defect mild or severe.
- Associated defects—is there another problem or a cluster of problems (syndrome).
Amniocentesis and/or microarray may be necessary for chromosome testing. Sonography is the best imaging tool, but is dependent on the experience and expertise of the operator. Magnetic resonance imaging may be necessary in some cases. Many problems are first detected during routine screening procedures performed in your doctor’s office (amniocentesis, maternal serum screening, routine sonography), but assessment of complex usually requires a tertiary perinatal/neonatal center with experience managing complex and rare fetal problems. We can work with your doctor to find a center convenient for you.
What are my choices during this pregnancy?
Most fetuses with pulmonary sequestrations do not require intervention during the pregnancy and will do well with management after birth (usually surgery to remove the abnormal piece of lung). Fetuses with pulmonary sequestrations, identified by an abnormal artery on ultrasound, usually do well with surgical removal after birth.
Fetal Intervention
A few fetuses develop fluid collections in the chest cavity which may be treated by draining the chest fluid into the amniotic fluid. Placement of a Harrison thoracoamniotic shunt involves a fetal procedure. A needle is guided through the maternal abdomen into the fetal chest. A cather is deployed and left in the fetal chest and drains the fluid into the amniotic fluid around the fetus.
Exit Procedure
If the fetus has a very large lesion that will make resuscitation after delivery dangerous, a specialized delivery can be planned called the EXIT (ex utero intrapartum treatment) procedure. We developed the EXIT procedure for management of fetal airway emergencies, but it can be adapted to facilitate immediate ECMO support or surgical resection of very large lesions while the baby remains attached to the placenta. This is rarely necessary for pulmonary sequestrations.
What will happen after birth?
Fetuses with small or moderate-sized pulmonary sequestrations that do not change much during pregnancy can be successfully managed after a normal birth. They usually do not have any difficulty during pregnancy or after birth. Unlike congenital pulmonary airways malformation (CPAM), all pulmonary sequestrations should be surgically removed because of the high blood flow through the lesion that can cause heart failure. This surgery is quite safe even in the first year of life and does not compromise lung function or the normal development of the baby. These children will grow up normally and have normal lung function.
Support Groups & Other Resources
- March of Dimes — Researchers, volunteers, educators, outreach workers and advocates working together to give all babies a fighting chance
- Birth Defect Research for Children — a parent networking service that connects families who have children with the same birth defects
- Kids Health — doctor-approved health information about children from before birth through adolescence
- CDC - Birth Defects — Dept. of Health & Human Services, Centers for Disease Control and Prevention
- NIH - Office of Rare Diseases — National Inst. of Health - Office of Rare Diseases
- North American Fetal Therapy Network — NAFTNet (the North American Fetal Therapy Network) is a voluntary association of medical centers in the United States and Canada with established expertise in fetal surgery and other forms of multidisciplinary care for complex disorders of the fetus.