The Fetal Treatment Center work directly with members of the UCSF Fetal Cardiovascular Program in the diagnosis and treatment of fetal congenital diseases.
What is congenital heart disease?
Fetal congenital heart disease involves an abnormality of the heart, whether it is a structural defect, a problem with the fetal heartbeat, or a functional problem with the heart squeeze or filling.
The fetal heart starts as a tube which folds and fuses in a complex dance that results in a muscular pump with four chambers and four valves. It is not surprising that small errors in development can lead to a wide variety of structural abnormalities in the 4 chambers, the 4 heart valves, the veins and great arteries. Most common heart defects, such as holes between the chambers (atrial septal defect, ventricular septal defect) and even more complex conditions such as transposition of the great arteries and tetralogy of Fallot, can be successfully managed after birth.
There are also a few structural abnormalities (such as narrowing of a valve) that can interfere with development of the pumping chambers, which can be very difficult to fix after birth. For instance, severe obstruction of the aortic valve, the outlet valve through which the left ventricle pumps blood to the body, may lead to poor growth and function of the left ventricle and other left heart structures. Ultimately this may result in the development of “hypoplastic left heart syndrome,” one of the most serious and common heart defects we encounter in sick newborns. In these cases, relief of the obstruction while the baby is still in the womb may allow more normal development of the ventricle, thus resulting in a very different outlook for the infant after birth. In the same way, narrowing of the pulmonary valve can damage the developing right ventricle or pumping chamber that normally pumps to the lungs. Abnormal development of either one of the pumping chambers (right or left ventricle) can lead to devastating problems after birth, which often require multiple complex open heart surgeries and, even when successful, result in distinctly abnormal function (so-called ‘single ventricle physiology’).
Abnormalities of the heart’s conduction system can result in abnormalities of the heart rhythm referred to as “dysrhythmias” or “arrhythmias”.
Heart abnormalities can now be accurately diagnosed before birth by fetal echocardiography. In most cases, this leads to improved postnatal management. In a few cases, it may also allow for fetal intervention—such as opening up an obstructed valve (and thus prevent abnormal development of the pumping chamber) or treating abnormalities of the fetal heart rhythm in utero by administering medications to the pregnant mother.
More information from the American Heart Association
For specific information about congenital heart disease we recommend the Health Topic guides on the American Heart Association
What is fetal dysrhythmia or arrhythmia?
Congenital heart disease may also involve the conduction system of the heart, which is responsible for making the heart beat at a normal rate.
Abnormalities of the conduction system cannot be seen with ultrasound, but the resultant abnormalities in the rate at which the heart beats can be easily diagnosed in an experienced center. The heartbeat of a normal, healthy fetus ranges between 120-160 beats per minute and has a regular rhythm. When the rhythm is irregular, or the heartbeat is too fast or too slow this is considered a “dysrhythmia” or “arrhythmia.” While most irregular rhythms do not get a baby into trouble before birth, fast or slow rhythm disturbances can cause the baby to develop heart failure and even die before birth.
One of the most common abnormal rhythms is “supraventricular tachycardia” in which the fetal heartbeat is very fast, at times even double the normal heart rate. Supraventricular tachycardia can be fatal to the fetus but if treated can be controlled or cured with a very good outcome. The treatment primarily involves giving one medication or more to the mother that cross through the placenta to the baby, and corrects the abnormal rhythm. Proper treatment requires knowledge about the kind of abnormal rhythms that may present in the fetus and the specific medications, including their doses, that are most likely to convert the baby’s abnormal rhythm to a normal rhythm and heart rate without causing any harm to the mother. Even with conversion of the rhythm to a normal rhythm, delivery at a tertiary care center where the baby can be managed after birth by individuals experienced in rhythm disturbances in newborns is usually required.
Another problem with fetal heart rate and rhythm that is diagnosed before birth is fetal bradycardia. Fetal “heart block” which occurs in varying degrees but at its most severe can result in a heart rate that is too slow to sustain the life of the fetus. When heart block occurs in isolation, it may be associated with abnormal factors, known as antibodies, which pass through the placenta from the mother and alter the conduction system of the fetal heart. Through the use of medications that reduce inflammation and increase the baby’s heart rate as well as close monitoring and early delivery when necessary, we have significantly improved the survival and outcome of these babies.
What causes problems with the fetal heart function?
Before birth, babies can develop problems with the function of the heart, including its ability to fill and to eject blood to the body and back to the placenta. This may be due to primary problems with the muscle of the heart itself known as “cardiomyopathies” or may be secondary to added stress on the heart from other problems such as structural heart defects, rhythm disturbances, defects that compress the heart and do not allow it to fill normally (e.g. congenital cystic adenomatoid malformation) or problems that result in increased work of the heart, (e.g. fetal anemia, acardiac twins, sacrococcygeal teratomas and other arteriovenous malformations, and twin-to-twin transfusion syndrome). For some of these conditions, there are ways to intervene before birth to improve the heart function and the baby’s overall outlook. Fetal echocardiography can help to identify those babies in whom intervention should be provided before birth, determine the best timing for intervention, and assists in determining how effective the intervention has been.
What is the outcome for a fetus with congenital heart disease?
The outcome for the fetus diagnosed with heart disease depends in a large part on what the precise problem is, and also on whether there are any other non-cardiac abnormalities present. Most structural congenital heart defects can be addressed after birth with excellent results. Some may not need any intervention, some may require a single surgical or interventional catheterization intervention, and some may require two or more surgeries.
However, a few severe defects, such as those that lead to maldevelopment of one of the pumping chambers, may not be correctable after birth, or may require a series of open heart surgeries that, even if successful, result in abnormal circulation (single ventricle physiology) and life-long limitations. Rhythm abnormalities, if treated early and successfully in the pregnancy, generally have very good outcomes—many fetuses treated in utero for tachyarrhythmias do not require any intervention after birth and may not even need medication after the first few months of life.
There is, however, a range of outcomes for fetuses with congenital heart disease that are treated after birth, therefore for the few fetuses with distinct structural defects that lead to death or life-long difficulty, fetal surgical intervention may be an option. For detail on fetal intervention for congenital heart disease visit our Treatment page or download our PDF Brochure about Fetal Intervention for Congenital Heart Disease.
How serious is my fetus’s congenital heart disease?
When fetal heart disease is suspected, it is very important that a complete, thorough evaluation be undertaken prior to discussing the implications. Co-occurrence of additional subtle valve abnormalities with a septal defect, for instance, may have important implications for the postnatal management and surgical interventions for the child. Fortunately, fetal echocardiography has improved dramatically over the last decade, so that most abnormalities, even subtle anatomic variations, can be completely and accurately diagnosed by an experienced fetal echocardiographer/cardiologist. This often requires evaluation at a tertiary or quaternary fetal echocardiography center.
Echocardiography will determine whether your fetus has the type of structural abnormality that can be successfully repaired after birth, a rhythm abnormality that can be treated before birth, or the unusual type of structural problem that might make your fetus a candidate for fetal intervention: for example, critical aortic stenosis (narrowing of the aortic valve) with evidence of developing hypoplastic left heart syndrome, critical pulmonic stenosis (narrowing of the pulmonic valve) with evidence of ongoing damage to the right side of the heart, or restrictive atrial septum (early closure of a flap valve in the fetal heart) leading to abnormal pressure in the fetal veins.
What are my choices during pregnancy?
Once the diagnostic evaluation has been completed, there may be several options to be considered by the patient/family. The available options depend on the specific congenital heart disease, and should be discussed with the patient by someone with training and experience in treating infants and children with heart disease. For some, fetal intervention or treatment may be an option. For some, if fetal or newborn intervention is not necessary, returning to their referring obstetrician and delivering in their local community may be preferable.
There are on the other hand a number of complex heart defects that will not benefit from intervention before birth, but will benefit greatly from prenatal diagnosis and management at an appropriate tertiary referral center. Many of these defects were life-threatening in past decades (before advances in newborn care of infants with congenital heart disease were developed) but now can be very successfully corrected shortly after birth. Some will benefit from being delivered at the tertiary center, while others can be safely transported to the tertiary center after being born elsewhere.
Many families will want to work out a plan for delivery and postnatal care with their obstetrician/perinatologist, pediatric cardiologist, and pediatric cardiac surgeon, so the baby can be stabilized and treated in the same center. Diagnosis of the heart defects before birth allows us to inform the patient/family and plan for the delivery of the baby to give the baby the best chance at a good outcome.
Fetal Intervention
For fetuses earlier in gestation who have not already developed severe damage to the ventricular wall with underdevelopment of the heart on the side of the obstruction, intervention to dilate or enlarge the obstructed valve may be considered.
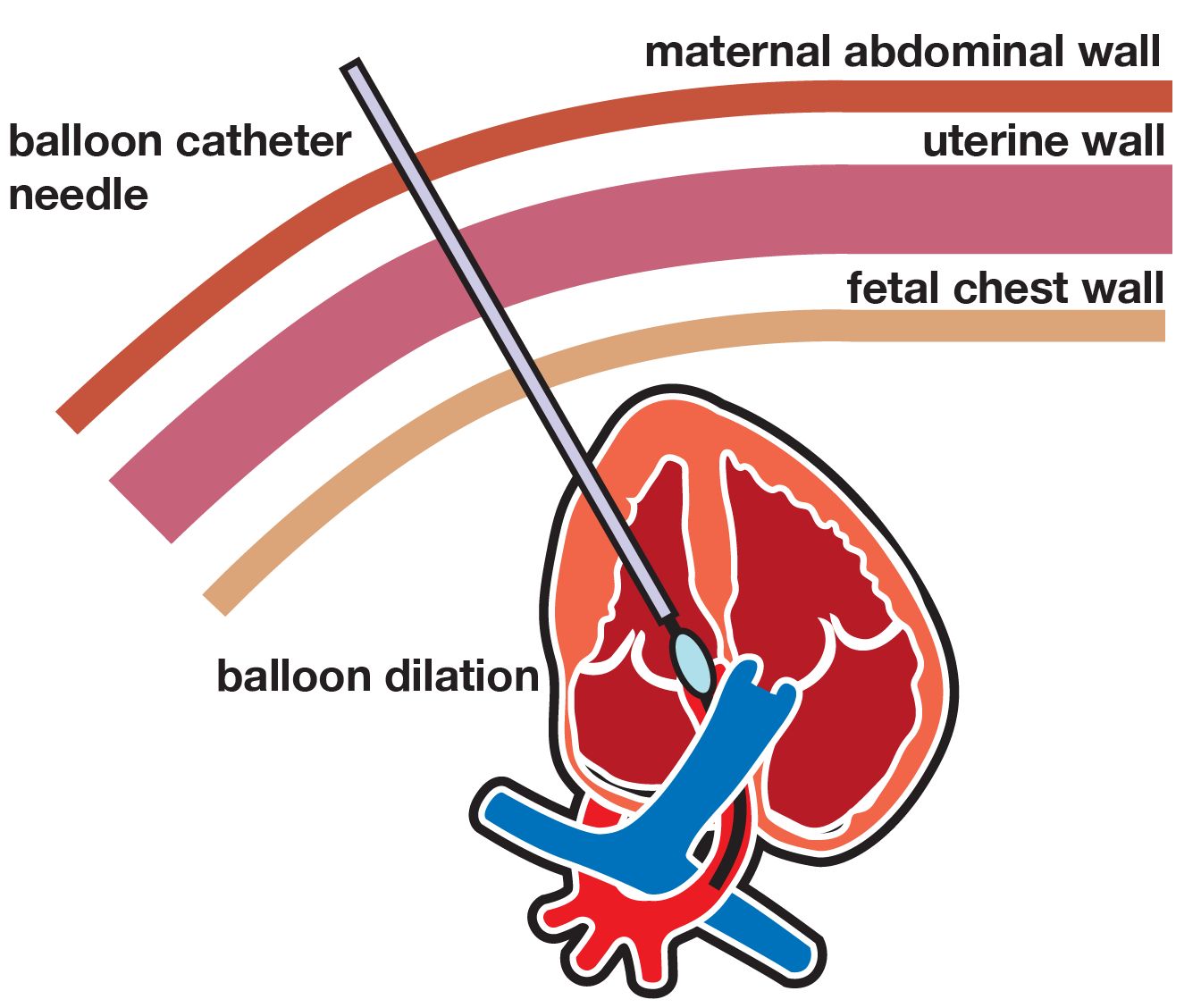
An obstructed outlet valve can be dilated using a balloon catheter placed into the fetal heart through the mother’s abdominal wall, using Fetal Image-Guided Surgery (FIGS-IT), or through the uterine wall after opening the mother’s abdomen.
For more information please visit ClinicalTrials.gov to learn about our ongoing clinical trial.
Support Groups & Other Resources
- CHD Care Compass — empowering families with knowledge and tools for the CHD care journey
- Fetal Heart Society — advancing the art and science of fetal cardiovascular medicine
- Hearts Unite the Globe — devoted to providing information to members of the world-wide congenital heart defect (CHD) community
- March of Dimes — researchers, volunteers, educators, outreach workers and advocates working together to give all babies a fighting chance
- Birth Defect Research for Children — a parent networking service that connects families who have children with the same birth defects
- Kids Health — doctor-approved health information about children from before birth through adolescence
- CDC - Birth Defects — Dept. of Health & Human Services, Centers for Disease Control and Prevention
- NIH - Office of Rare Diseases — National Inst. of Health - Office of Rare Diseases
- North American Fetal Therapy Network — NAFTNet (the North American Fetal Therapy Network) is a voluntary association of medical centers in the United States and Canada with established expertise in fetal surgery and other forms of multidisciplinary care for complex disorders of the fetus.