What is Spina Bifida (Myelomeningocele)?
Spina bifida is a congenital defect consisting of an opening in the spinal column. The most severe form is called myelomeningocele. Most children with this birth defect survive, but they can be left with many disabilities, including paralysis, difficulty with bowel and bladder control, a Chiari II malformation, hydrocephalus (excessive fluid in the brain), and developmental delay. In general, the higher the spinal opening occurs on the back, the greater the physical impairment.
Treatment for Myelomeningocele
Infants with myelomeningocele have always had surgery shortly after birth to protect the spinal cord by closing the normal tissues of the back. Very often, a ventriculoperitoneal (VP) shunt was also placed to treat hydrocephalus. Due to the success of the MOMS Study, fetal surgery is now considered to be a treatment option for some cases of myelomeningocele.
Download our handout on Fetal Surgical Repair of Myelomeningocele PDF
Fetal Surgery for Myelomeningocele
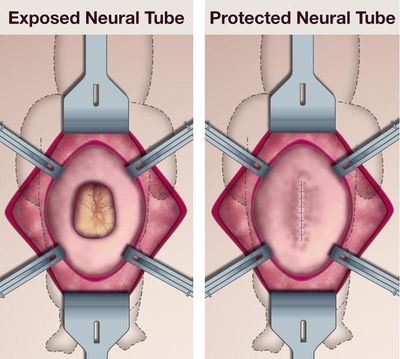
Prenatal repair of myelomeningocele involves a fetal surgery handled by a multidisciplinary team of experts. The procedure is much like a cesarean section however the fetus is not removed and the umbilical cord is not touched. An incision is made in the mother’s abdomen and uterus just large enough for the spinal defect to be operated upon. The neural tube and other layers of the back are surgically closed by the neurosurgeon. After the procedure, the incisions in the mother are closed.
Recovery From Your Operation
After the procedure, patients will remain in the hospital for 4–5 days for recovery. They are cared for by skilled nurses with years of experience in fetal surgical care and the fetus will be monitored via ultrasound. Upon hospital discharge the mother is required to stay locally for at least 2-3 weeks. Travel home is determined by the mother's condition and the availability of medical services.
Evaluation and Counseling
Components of UCSF Evaluation
- Level II anatomic survey for fetal anomalies
- Fetal echocardiagraphy both for the structural integrity and functional pathology
- Fetal brain MRI and spine for presence and severity of the Chiari II Malformation
- Consultations with our multidisciplinary team including anesthesia, fetal surgery, neurosurgery, nursing, perinatology, and social work
Guidelines For Fetal Surgery
Fetal surgery can be a treatment option for spina bifida. We have developed the following guidelines to determine fetal surgery candidates.
Inclusion Guidelines
- Myelomeningocele defect must start between T1-S1 (may extend below S1)
- Chiari II malformation diagnosed by MRI
- Normal fetal karyotype (amniocentesis)
- Gestational age at referral between 19 to 26 weeks
Exclusion Guidelines
- Multifetal pregnancy (twins, triplets, etc)
- Maternal contraindications to surgery or anesthesia
- Body Mass Index > 35
- Kyphosis (curve in the spine) in the fetus ≥ 30º
- Other fetal problem not related to the spina bifida
- Current or planned cerclage or documented history of incompetent cervix
- Short cervix (> 20 mm)
- Preterm labor in the current pregnancy
- Placenta previa or placental abruption
- Maternal-fetal isoimmuization
- Uterine abnormality
- Inability to comply with travel or follow-up requirements
How to Make an Appointment or Referral
Patients who wish to consider fetal surgery at UCSF for the treatment of spina bifida, and providers making a referral please use our online appointment form or call us at 1-800-RX-FETUS. Also please have the following information faxed to 415-502-0660:
Name, home address, phone, email, date of birth
Copy of the front/back of their health insurance card
All OB/Perinatal medical records
If insurance authorization is required, please download the Spina Bifida Fetal Surgery FTC Codes.